Content:
- What is Cirrhosis?
- Morphological features
- Classification
- Causes
- Clinical manifestations/Symptoms
- Pathogenesis
What is Cirrhosis?
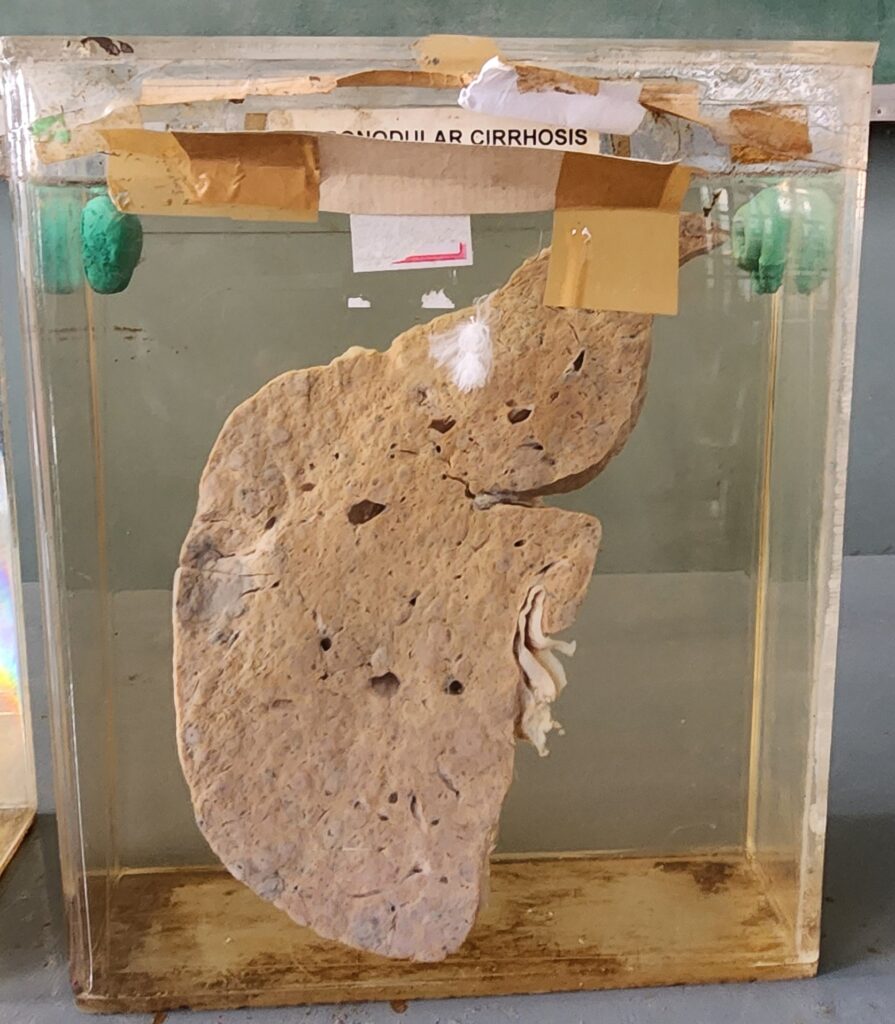
Cirrhosis is the terminal stage of CHRONIC LIVER DISEASE, in which the entire liver is involved. It is characterised by fibrosis and remodeling of the entire liver into parenchymal nodules (small swelling or aggregation of cells, especially abnormal ones) which are often regenerative. These nodules are surrounded by fibrous bands and a variable degree of vascular shunting. Cirrhosis and chronic liver failure are often associated but not all end stage chronic liver diseases are cirrhotic, similarly not all cirrhosis leads to chronic liver failure.
Morphological features:
1.Fibrosis: Here, the fibrous tissue form delicate bands or broad scars and link portal tracts with one another and portal tracts with hepatic vein. (*portal tract: portal tracts or portal triad is a distinct anatomical feature in the liver, which comprises of three main structures i.e., hepatic artery, portal vein and bile duct. Hepatic artery supplies oxygenated blood to the liver, portal vein brings nutrient rich blood from the gastrointestinal tract to the liver and bile duct carries bile produced by the liver to the gall bladder and small intestine)
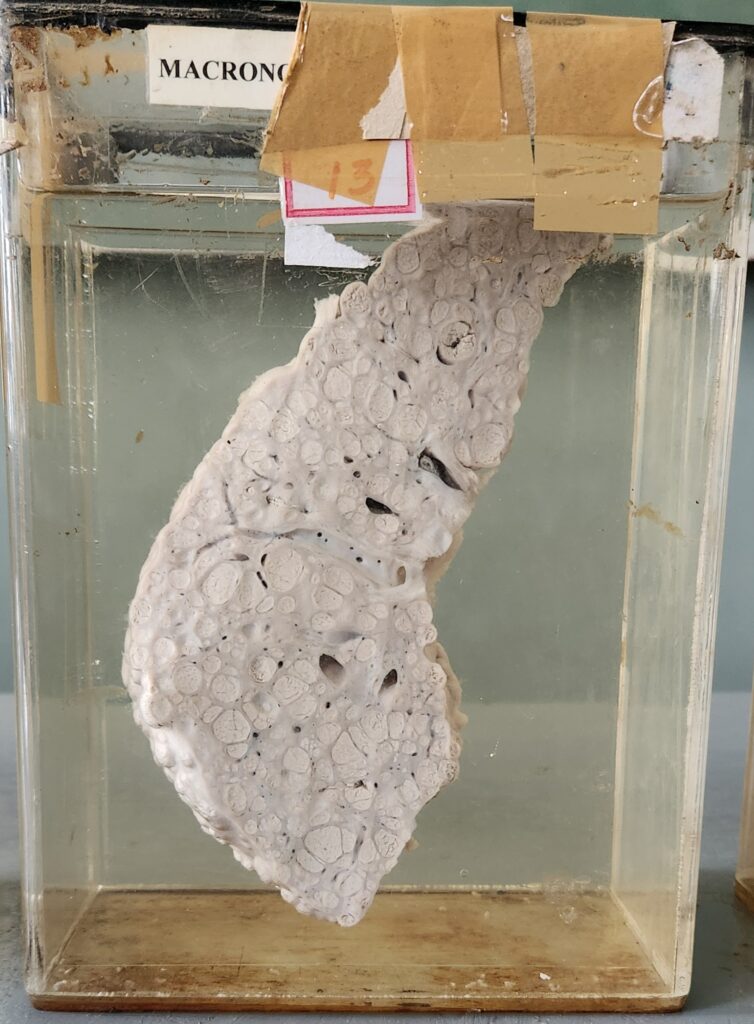
2. Regenerating nodules: Cirrhosis is marked by the presence of parenchymal nodules surrounded by dense bands of fibrosis throughout the liver, converting the normally smooth liver capsule into a bumpy surface with depressed areas of scaring and bulging regenerative nodules. This development of nodules is a form of compensatory mechanism by the hepatocytes (liver cells) against the liver cell damage.
3. Loss of Architecture: The fibrosis and nodulation occur throughout the whole liver and there by destroy the normal architecture of the liver.
Classification of cirrhosis:
Depending on the size of nodules, cirrhosis can be classified into three subtypes,
i. micronodular
ii. macronodular
iii. mixed
i. Micronodular: Here, small and regular nodules are present which measure less than 3 mm in diameter.The fibrous tissue septa are usually thin. Eg; alcoholic cirrhosis
ii. Macronodular: Here, nodules of variable size are present, also these are irregular in pattern. The nodules measure more than 3 mm in diameter. The fibrous tissue septa us broad. Micronodular cirrhosis can be converted into a macronodular form by continued regeneration and expansion of existing nodules. The macronodular cirrhosis has an increased risk of developing carcinoma of lover. Eg; cirrhosis associated with chronic hepatitis.
iii. Mixed: Shows features of both micronodular and macronodular cirrhosis.
Major causes of Cirrhosis:
- Alcohol is one of the most common causes.
- viral hepatitis
- Hemochromatosis which is excessive accumulation of body iron.
- Autoimmune liver disease
- Biliary obstruction eg; gallstones
- Wilson’s disease (progressive accumulation of toxic levels of copper in liver and various other tissues)
- Drugs and toxins
- Cryptogenic (hidden cause) or idiopathic (cause unknown)
Clinical manifestations/symptoms:
- Initially the patients are asymptomatic and this phase is called “compensated” cirrhosis.
- Later the patient presents with complications associated with portal hypertension or liver dysfunction.
Non-specific clinical manifestations are:
- Anorexia (eating disorder characterised by a low body weight, intense fear of gaining weight and a distorted perception of body weight)
- Weight loss
- Weakness, fatigue
- Vomiting
- Low grade fever
- Abdominal distension (swelling) due to ascites and gas
- Loss of libido
- Menstrual irregularities like anenorrhoea and irregular menses
- Hemorrhagic tendencies like easy bruising, purpura, epistaxis, menorrhagia (heavy or prolonged menstrual bleeding) and gastrointestinal bleeding. Hemorrhagic (excessive bleeding) tendencies are due to underproduction of blood coagulation factors by the liver and thrombocytopenia resulting from hypersplenism.
Pathogenesis:
Cirrhosis involves four important processes.
- Death of liver cells leading to loss of Architecture of liver. Alcohol is a direct hepatotoxic and it’s metabolism in the liver initiates many pathologenic process. About 10-15% of alcoholics develop cirrhosis. The oxidation of ethanol produces several toxic agents and damages the metabolic pathways.
- Fibrosis: One of the characteristic feature of cirrhosis is fibrosis. Alcohol activates hepatic stellate cells transforming them into highly fibrogenic cells with myofibroblast-like contractile property which produce collagen and lose their stored vitamin A. (*Stellate cells are present in the space of Disse between hepatocytes and sinusoidal endothelial cells. Normally, stellate cells are quiescent (in a state or period of inactivity or dormancy) and store vitamin A)
- Regenerating nodules: The liver cell damage and fibrosis stimulates the surviving hepatocytes to regenerate and proliferate, forming regenerative nodules surrounded by fibrous septa. The regeneration nodules lack the normal structure of the liver lobules or acini.
- Vascular reorganisation: The parenchymal damage and fibrosis disrupt the vascular architecture of the liver. This causes new vascular channels to form in the fibrotic septa, which connect the hepatic artery and portal vein to terminal hepatic veins, shunting blood from the parenchyma.
Source:
- ROBBINS AND COTRAN – Pathologic basis of disease
- Ramdas Nayak and Rakshata Nayak – Exam preparatory manual for undergraduates (Pathology)
- K George Mathew and Praveen Aggarwal – Exam preparatory manual for undergraduates (Medicine)